Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Cutaneous and Mucous Sinus Tract of Dental Origin: What’s Behind it?
*Corresponding author:Brigui Fouad, Department of dentistry University of Monastir Dental Faculty of Monastir..
Received:April 04, 2023; Published:April 17, 2023
DOI: 10.34297/AJBSR.2023.18.002489
Abstract
Dental Sinus Tract is an inflammatory channel putting in communication a deep peri-dental suppurative lesion with an exit orifice, it’s nature’s method of establishing drainage. A general practitioner commonly encounters in his practice this type of lesion. However, their discovery is very often delayed due to their chronic nature (asymptomatic) and their localization (hidden in the mucous folds or in skin furrows). The aim of this clinical case reports is to dissect the diagnostic difficulties and to discuss the therapeutic particularities of the management of mucous and cutaneous fistulas of dental origin. the first patient was referred to our service for the extraction of an impacted canine in whom we discovered by chance a mucous fistula that hides a cystic lesion perforating the vestibular alveolar table, after 2 weeks of intracanal calcium hydroxide and a root canal obturation, periapical surgery was performed with apical resection and 3 mm MTA plug. the second patient was referred by the maxillofacial department to verify a possible dental origin for the drainage of the cutaneous sinus tract in the left posterior part of the cheek, the radiographic analysis shows a decayed 36 with diffuse radiolucency and a resorbed distal root. The tooth was judged to be preserved and after root canal instrumentation and calcium hydroxide medication, the skin lesion shows signs of healing, therefore, the root canal filling was made with a bio-ceramic sealer and the patient was put under control. The key to the success of the treatment of mucous and cutaneous sinus tract of dental origin is, first of all, to know how to identify the etiology to their existence in order to not misdiagnose and initiate inappropriate therapies and, secondly, to be aware of the importance of post-operative follow-up. Finally, the treatment of the dental cause, conservative or not, leads generally to the disappearance of the fistula and a regression of the symptoms.
Keywords: Sinus tract, Endodontic treatment, Extra oral cutaneous fistula
Introduction
Dental Sinus Tract - from the Latin “fistula”, is an inflammatory channel putting in communication a deep peri-dental suppurative lesion with an exit orifice, it’s nature’s method of establishing drainage [1]. A general practitioner commonly encounters in his practice this type of lesion. However, their discovery is very often delayed due to their chronic nature (asymptomatic) and their localization (hidden in the mucous folds or in skin furrows) [2]. The fistula follows a suppurating process which is the consequence either of a dental pathology or of a periodontal pathology and this process follows a very brief acute mode or a chronic mode which warms up and follows the first mode [2]. The aim of this clinical case reports is to dissect the diagnostic difficulties and to discuss the therapeutic particularities of the management of mucous and cutaneous fistulas of dental origin.
Cases Report
First Case Presentation
43-year-old patient “Z.S” with no medical or surgical history was referred for surgical extraction of the impacted canine, the patient reports no history of pain. Clinical examination reveals the presence of a generalized fluorosis which camouflages the dyschromia of the 11 and the presence of a mucosal fistula regarding the apex of tooth 11 (Figure 1). The tooth was free of caries with normal periodontal probing. Pulp sensitivity test and percussion were negative, the realization of intra- oral radio with gutta-percha (25/04) traces the fistulous path cord and connects the orifice to an the indicated treatment was an endodontic treatment by insisting on the canal paring, then, a periapical surgery. The tooth was free of caries with normal periodontal probing. Pulp sensitivity test and percussion were negative, the realization of intra- oral radio with gutta-percha (25/04) traces the fistulous path cord and connects the orifice to an image of osteolysis which caps the apex of the 11, the radio revealed an intimate relationship between the periapical lesion and the peri coronal sac of the impacted canine thought (Figure 2,3).
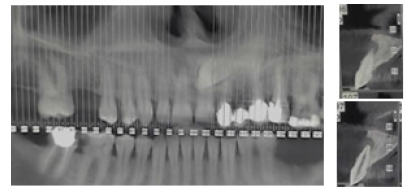
Figure 3:Cone-beam computed tomography showing no intimate relationship between impacted canine and cystic periapical lesion of 11.
At first impression, it was thought that the peri coronal sac of the canine was responsible for the necrosis and the periapical complication of the 11. Following the cone beam analysis, it turned out that the relationship with the canine was not intimate and that the apex of 11 was capped with a cystic-looking image that perforates the vestibular alveolar table. The interrogation reveals that the patient has been a brux addict for several years without any history of trauma, in addition, zooming in on the crown of the 11th shows the presence of vertical buccal crack, several palates cracks and abrasion surfaces (Figure 4). Therefore, the pulp necrosis is the consequence of the coronary cracks (long process) and a diagnosis of fistulized apical abscess was made. The indicated treatment was an endodontic treatment by insisting on the canal paring, then, a periapical surgery.
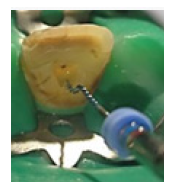
At the First Session
The access cavity was carried out, complete shaping with mechanical activation of CLONA 5.25% and EDTA 17% using FKG’s EX endo shaper and hydroxide-based medication of calcium mixed with chlorhexidine was placed inside the root canal (Figure 5,6,7).
At the Second Session (After 2 Week)
The clinical control highlights the disappearance of the fistula and an asymptomatic tooth (Figure 8,9). The canal obturation was made with a single Gutta-Percha cone and bio-ceramic (CERASEAL) as sealing cement (Figure 9).
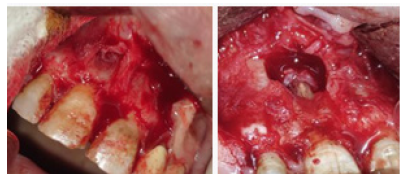
At the Third Session (After 2 Week)
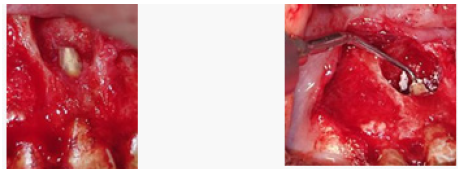
Cystic enucleation was performed after a full-thickness flap lift. the apical resection was made at 0° angle with the ZEKRIA bur, then the 3mm intracanal preparation for the MTA plug was made with an angled ultrasonic tip. (Figure 10,11,12).
Second Case Presentation
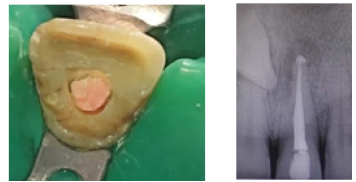
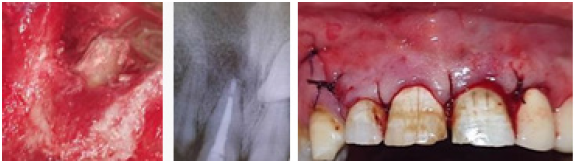
A healthy 16-year-old male patient was referred by a maxillofacial practitioner to verify a possible dental origin for draining cutaneous sinus tract in the left posterior portion of the cheek. During history taking, the patient reported that there had been intermittent drainage from the fistula for 3 months. The patient complains a lot of aesthetic discomfort. Extraoral examination disclosed no abnormalities except for an erythematous area, approximately 2 cm in diameter, above the inferior border of the mandible. A red cutaneous depression was visible in the center of this area. Moderate pressure produced a discharge of pus and serous fluid, palpation can identify a cord connecting the mandible to the soft and painless skin. The patient reported that there had been intermittent drainage from this area for more than 3 months (Figure 13). The clinical examination reveals a necrotic first left mandibular molar following a large carious lesion with pulp exposure. A Periapical radiograph revealed a 5 mm (diameter) radiolucent area associated with the mesial and distal apices of this tooth. A severe distal root external resorption was mentioned. A clinical diagnosis of chronic alveolar abscess was made (Figure 14,15).

Figure 13:Preoperative extra oral view of the draining cutaneous sinus tract in the left posterior portion of the cheek.

Figure 14:Preoperative intra oral view showed the left mandibular first molar (tooth 36) after removing the decayed tissue. The gum and apical mucosa of were normal without red and swollen.

Figure 15:Preoperative x-ray of the left mandibular molar showing diffuse radiolucency associated with the mesial and distal.
At the First Session
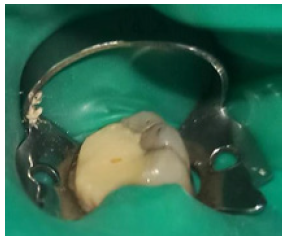
After carious curettage and pre-endodontic restauration were performed (Figure 16), root canal therapy was initiated with pulp chamber access and biomechanical preparation. Irrigation during instrumentation was carried out with 2.5 % sodium hypochlorite and final irrigation with 17 % EDTA solution, which remained for 2 min in the canals. Calcium hydroxide paste was used as the intracanal medicament. The access cavity was sealed with glass ionomer cement.
At the Second Session
After 2-week, drainage through the fistula had ceased (Figure 17). The lesion appeared to be in the first stage of healing, the prior depression aspect decreased. The root canal obturation was completed with a master gutta-percha cone and a bioceramic endodontic sealer (BioRoot™ RCS) (Figure18,19).

Figure 17:Obvious signs of initial healing of the fistula after 2 weeks later after root canal therapy and Ca(OH)2 medication.
One Month Later
Without surgical treatment, the cutaneous fistula continues healing with deep skin adhesions resulting in an unsightly umbilical scar. The patient was symptom free (Figure 20).
Discussion
Identification of the Causative Tooth
Mucous Sinus Tract: The fistula is a lethen with very little signs and symptoms because of the fact that drainage of the periapical collection is ensured, consequently the phenomenon of chronic abscess can stay silent for a protracted duration. [3,2] During clinical examination and identification of the causative tooth, we may find different situations in the simplest case, the causal tooth is necrotic (decay / trauma / periodontal problem) with a radiolucent periapical image, an X-ray gutta percha placed in the fistulous path confirms the etiology with certainty (the case of the first clinical situation). Sometimes it is difficult to determine whether it is of periapical, periodontal, or periosteal origin, even when radiolucencies are found around or over teeth. Negative radiographic findings make this differentiation even more difficult. The location of the fistulous opening, of itself, is often misleading as to which tooth or tissue is involved. The fistulous opening does not necessarily break through the soft tissue over the involved tooth. Exudate burrows its way sometimes for great distances before it is discharged. Therefore, it is necessary to know the origin of the fistula in order to institute proper treatment [2,4]. In chronic apical inflammatory lesions, a fistula may be gift without any radiographic evidence of periapical involvement. That is because of the presence of a thin labial plate of cortical bone that has been eroded over the apex of the tooth due to the inflammation. No longer sufficient cortical bone is destroyed to supply a detectable contrast on the roentgenogram [1]. In instances in which one tooth exhibits periapical involvement in the roentgenogram and a fistula is present, the fistula is normally the result of that periapical involvement. But it isn’t always necessarily the case in all times. On occasion, the fistula may be due to periodontal involvement, in spite of the presence of the apical radiographic rarefaction. It is requisite, therefore, to determine whether the fistula is of periapical or periodontal starting, so that correct treatment may be instituted [1].
Diagnosis is facilitated by using a fine stainless-steel orthodontic ligature wire, 0.01 in thickness. This may be introduced, without problems, into the orifice of the fistula; then, with an easy, twirling movement and really light strain, the entire fistulous tract can be negotiated. False communication is difficult to set up and any resistance may be felt. Even as gutta-percha points have been advised previously for differential analysis, they’re no longer as correct or adaptable because the thin orthodontic cord [5]. In some of instances, a fistula can be present among two tooth, both of which show areas of rarefaction in the radiograph. Right here, the wire approach is highly recommended. The wire is inserted into the fluctuant area and, maneuvered with an easy, twirling motion, it’s going to negotiate the inflammatory path to the causative tooth. The presence of a fistula close to an endodontically treated tooth does no longer always imply that the tooth is apically involved as a result of improper endodontic treatment. The fistula could rise from a periodontal involvement of the same tooth. The wire communicates with the area of rarefaction which has resulted from the periodontal disturbance [6].
Cutaneous Sinus Tract: Cutaneous sinus tracts of dental origin still present a diagnostic challenge because they frequently have a scientific appearance similar to different facial lesions, which includes carcinomas, furuncles, osteomyelitis, bacterial infections, congenital fistulas, and pyogenic granulomas. So, a dental infection need to be suspected as the primary etiology in persistent draining cutaneous sinus tracts of the face and neck. This diagnosis would possibly easily be disregarded by physicians. Patients may consequently go through many irrelevant surgeries and guides of antibiotics before a definitive analysis is made and the appropriate remedy is initiated. [3,5] fortunately, our patient (second clinical case) was referred to our department by the maxillofacial department before any attempt at surgical excision. Tracing an endodontic gutta-percha point along the mucosal sinus tract through the radiographic examination can discover the affected tooth. But this isn’t evident with cutaneous sinus tracts because of the space among the orifice of the fistula and the alveolar bone as well as the presence of more than one range Cutaneous, muscular, and mucosal [7]. Radiographic examinations, traditional or advanced imaging, should be finished to become aware of any radiolucency on the apex of the suspected tooth. Those investigations are notably more critical if multiple teeth are suspected. For example, CBCT assist to identify the affected tooth and to reveal the presence of nearby perforation of the vestibular table, which cannot be shown by the traditional 2d radiography [3].
Treatment
Dental Etiology: It is necessary and almost sufficient to ensure the treatment of the dental cause to obtain the healing of the skin or mucous lesion. Necessary, because all antiseptic or antibiotic medical attempts, both local and general, can not ensure the disappearance of the fistula and will result only in a temporary reduction of the drainage and pseudo healing [8] (Cases with an intact immune system, without general signs, or other systemic manifestations that would require prophylactic antibiotic therapy). surgical attempts to excise the skin lesion, including the fistulous tract, are doomed to recurrence if the causal tooth is left in place. Sufficient, because only the treatment of the dental focus most of the time leads to the drying up and fast disappearance of the fistula. Once resolved, the fistula tends to disappear very quickly between 5 to 15 days [8,9]. Sometimes, Persistence of a small pimple which tends to go unnoticed after a few months. therefore, as it was in our two clinical cases, if the tooth can be preserved, after shaping the canal system, it is filled with calcium hydroxide mixed with 2% chlorhexidine (this combination has shown better efficacity on periapical lesions) [10,11]. For mucosal fistulas, some authors recommend root canal obturation in a single session but for cutaneous fistulas, they recommend permanent root canal obturation after 2 weeks of hydroxide-based medication.
Sinus Tract:Should the presence of an epithelial border lead to additional management? according to VIRE 1982 in the event of an old fistula with an epithelial border, it recommends carrying out its excision. Now, according to the majority of scientists. It is agreed that a simple etiological treatment (endodontic or extraction) is enough to make the cord disappear and that the excision of the fistula can cause an unsightly scar. On the other hand, local disinfection of the fistula with chlorhexidine is recommended by several authors. They recommend cleaning 4 times a day for 10 days. Other solutions have been cited such as Triclosan [10].
Evolution
The Non-Regression of a Fistula: If a mucous fistula does not heal, other etiologies should be sought such as fractures, skipped canals. If a cutaneous fistula does not heal after satisfactory endodontic treatment or extraction, it is carry out additional examinations using biopsies and microbiological samples. The most common cause of non-regression is actinomycosis. [4,11].
Unsightly Scars
The orifices of mucous fistulas heal completely without leaving any sequelae. If the fistula is recent, the cutaneous scar will be almost invisible (almost identical coloring, paler, supple and without deep adhesions). On the contrary, if the fistula is old, the fistula has been organized for a long time, hence adhesions of the skin to the deep planes giving an unsightly umbilical scar. in fact, insufficiently developed scar tissue cannot fill all the loss of substance, which causes a retracted scar [4,12]. The restorative surgery a second time can correct this unsightly sequelae. It’s about realizing excision then plastic surgery [3,13]. The second way of proceeding consists in carrying out, in addition to the etiological treatment, the excision of the fistula associated with skin plastic surgery. This preventive approach is little described in the literature. Both of these methods have been tested by McCLUER from 1961 with similar aesthetic results [14,15].
Conclusion
The dental etiology must always be evoked with regard to any skin lesion. The treatment of the dental cause, conservative or not, depending on the severity of the dental lesions, leads to the disappearance of the fistula and a regression of the symptoms. Locally, surgical treatment may be necessary to improve the aesthetic appearance.
Acknowledgements
None.
Conflict of Interest
No conflict of interest.
References
- Bender IB, Seltzer S (1961) The oral fistula: its diagnosis and treatment. Oral Surg Oral Med Oral Pathol 14(11): 1367-1376.
- Ghodsi Sz, Ghiasi M (2006) Two unusual cases of dental (periapical) infection. Dermatol Online J 12(4): 15.
- Kallel I, Moussaoui E, Kharret I, Saad A, Douki N, et al. (2021) Management of cutaneous sinus tract of odontogenic origin: Eighteen months follow-up. Journal of Conservative Dentistry 24(2): 223-227.
- Patni PM, Prashanth MB, Jain N, Patni JM (2010) Non- surgical management of an extraoral cutaneous sinus tract of odontogenic origin: An endodontic challenge. Endo (Lond Engl) 4: 285-291.
- Alshammari MA, Alzoubi FM (2023) Endodontic management of unusual extraoral cutaneous sinus tract. Saudi Endodontic Journal 13(1): 108.
- Iris Slutzky Goldberg, Igor Tsesis, Hagay Slutzky, Ilana Heling (2009) Odontogenic sinus tracts: a cohort study. Quintessence Int 40(1): 13-18.
- Nestor Cohenca DDS, Sunil Karni BDS, Ilan Rotstein DDS (2003) Extraoral Sinus Tract Misdiagnosed as an Endodontic Lesion. The American Association of Endodontists 29(12): 841-843.
- Al Obaida MI, Al Madi EM (2019) Cutaneous draining sinus tract of odontogenic origin. A case of chronic misdiagnosis. Saudi Med J 40: 292– 297.
- Aboalsamh D (2021) Non-Surgical endodontic treatment of extra-oral cutaneous sinus tract: Case reports. J Oral Health Dent Res 1(1): 1-4.
- Soares JA, de Carvalho FB, Pappen FG, Araújo GS, de Pontes Lima RK, et al. (2007) Conservative treatment of patients with periapical lesions associated with extraoral sinus tracts. Aust Endod J 33(3): 131-135.
- Saatchi M, Shokraneh A, Navaei H, Maracy MR, Shojaei H, et al. (2014) Antibacterial effect of calcium hydroxide combined with chlorhexidine on Enterococcus faecalis: a systematic review and meta-analysis. J Appl Oral Sci 22(5): 356-365.
- Chkoura A, Elwady W, Taleb B (2010) Surgical management of a cutaneous sinus tract: A case report and review of the literature. J Contemp Dent Pract 11(5): 049-055.
- Tidwell E, Jenkins Jd, Ellis Cd, B Hutson, R A Cederberg, et al. (1997) Cutaneous odontogenic sinus tract to the chin: a case report. Int Endod J 30(5): 352-355.
- Dincol ME, Yilmaz B, Ersev H, Mert Gunduz V, Arslanoglu B, et al. (2015) Treatment of extraoral cutaneous sinus tracts with non- surgical endodontic intervention: Report of six cases. J Istanb Univ Fac Dent 49: 35-40.
- Mccluer Cf (1961) Dental abscess with sinus tract formation. Arch Dermatol 83: 941-944.












 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.